Community First Strategy 2023

What is Community First?
North Lincolnshire’s Health and Wellbeing Board and Place Partnership has a focus and commitment to transforming the lives of people in North Lincolnshire through an integrated health and social care system. The Community First Strategy is North Lincolnshire’s plan for achieving this.
The Community First Strategy is transformational. Whilst national drivers such as the Health and Social Care Act 2022 and the Fuller Report highlight the importance of, and need for, health and social care integration, it is the action we take locally that will make this integration a reality.
The Community First Strategy is a key part of the action we are taking locally. It will achieve health and social care integration in North Lincolnshire, enabling people and ensuring that they get the right care, in the right place at the right time.
Based on prevention and enabling self-help, people will be able to act to keep themselves well, with the person and family will be at the heart of everything the health and social care system does.
Community First will make it easy for communities to help people in ways that reduces their need for more health or social care and support. It will achieve this through:
- Offering health and social care services that work together and meet need, and
- Enabling communities by building the right capacity within communities so that they can support themselves.
Our shared ambition
Our ambition is for North Lincolnshire to be the best place for all our residents to be safe, well, prosperous and connected; experiencing better health and wellbeing.
This means that people will:
- Enjoy good health and wellbeing at any age and for their lifetime
- Live fulfilled lives in a secure place they can call home
- Have equality of opportunity to improve their health, play an active part in their community and enjoy purpose within their lives.

Our approach – Community First
Our approach to transformation empowers people of all ages, including children and young individuals, to actively engage in their own communities and their own wellbeing. This means that we place a strong emphasis on involving people and communities in health and care decisions.
We want to provide personalised care that allows individuals to take care of themselves and have more control over their lives. Our goal is to offer the best possible care as close to people’s homes as we can. To achieve this, we’ll use our collective resources to improve outcomes for people, taking into account the input and perspectives of our diverse communities.
We plan to utilise the assets and resources available in our local areas to focus on preventing health issues and providing community support. This way, we can reduce the need for more in depth levels of care. Our aim is to make sure that care is safe, effective, and of high quality, delivered in the right place and at the right time.
We will manage our resources responsibly and ethically, ensuring that the North Lincolnshire pound is used wisely. Participation and prevention will be integral to everything we do. We will build a united team culture and support our workforce in achieving positive outcomes for people, while also taking care of their well-being. We’ll make sure that our systems and tools for change are efficient and effective.
The Integrated Care System (ICS) will invest locally to make this vision a reality. Our goal is to create a community health and care system that is well-suited to the population’s needs, addresses inequalities, and emphasises prevention at all levels. We will also use digital tools to support individuals and facilitate collaboration among the workforce.
We will focus on those who need care the most and work together to manage risks effectively. By encouraging positive risk-taking, we aim to improve the outcomes we’re striving for.
What difference will Community First make?
We recognise that local leaders have the opportunity at Place to consider and design our own plan for integration – one that we can own, design and deliver for the people of North Lincolnshire. Our Community First Strategy is centered around the following outcomes:
- People are safe and have good quality provision
- People have urgent needs met quickly
- People are enabled to keep well
- Community
- Person and family.

The Person and Family are at the heart of everything we do.
Across North Lincolnshire all organisations involved in health and social care will work together to enable people to live independently within their own homes, families, jobs, schools and communities. This is important because it helps people to enjoy a better sense of wellbeing and keeps them close to the people that matter.
Community is at the very heart of our wellbeing
We will make sure people get the information, advice, guidance and help to keep themselves well and we will support carers to enjoy good health and wellbeing whilst continuing to care for their loved ones. We will make sure they get this from, and within, their communities. We will use what we know about the needs of people and the communities they live in to shape and target the way in which this help is designed and delivered.
People are enabled to keep well.
We have committed to prioritise prevention and early help and to do this we will develop Integrated Neighbourhood Teams which will ensure a fully integrated response across health, social care, housing, employment and voluntary sectors. Integrated Neighbourhood Teams will be proactive in identifying people with, or at risk of developing, long term conditions and or disabilities, and for those who have existing conditions, will provide them and their carers with high-quality, person-centered care. This will include assessment of need, good care planning and coordination that enables self-care, better and faster access to local solutions and support reduction in the need for urgent care. This will support people to remain in their own homes, communities, families, schools and employment.
Many people will have social, psychological, economic and environmental factors that cause additional complexities to their needs and therefore this will be underpinned by a population health management approach to target our interventions most effectively, including a holistic assessment based on a sociomedical care model.
People will have urgent needs met quickly
By establishing our unplanned care response into a fully Integrated Urgent Care system wide approach. We understand that some people do get into crisis at times and what they need more than anything is a rapid response, but one that is aimed at enabling that person to remain in their current environment and retain their independence, choice and control over what happens will mean that they are more likely to recover quickly and not ‘decondition’ in hospitals or care facilities.
If a person has a need for urgent care, our workforce will work together so that the person gets the care they need through one single point of contact. The care they get will feel seamless to them, and wherever possible the person will get the care within their community.
Hospital and care home admissions will be minimised and if people are admitted to hospital or care homes, the time that people spend there will be minimised, with people returning to their homes supported with the right care. Our staff will work together enable people to live independently within families and communities.
People will be safe and have good quality provision.
We have agreed we will have a single Integrated Strategic Commissioning and Safeguarding approach that maximises Place resources to best effect to meet need and achieve the best quality of provision for residents and that focuses on those who are most vulnerable. We will make the best use of resources, doing it once doing it well in terms of strategic planning and managing the commissioned services transformation together as one team. We will work together to coproduce and commission appropriate arrangements for people with complex needs and to support the health and care sector to deliver their best in meeting those needs.
Focusing on these outcomes for our plans for integration as described above will enable us to deliver improvements in nine areas of collective focus for our system:
- Mental Health and wellbeing will thread through all that we do across all ages
- Asset based community development will identify and work with the strengths of communities to level up North Lincolnshire
- Innovation will be supported including digital tools that enable individuals to maximise their health and wellbeing
- The health inequalities gap will reduce across all of our wards
- Healthy life expectancy will improve for our population
- Access to health and care will take account of rural challenges
- People with long term conditions such and lung and heart disease will experience proportionately better health
- There will be a single workforce strategy covering leadership and management, recruitment and retention, reward and recognition, career pathways and talent development
- The integrated practice model will be person centered.


Experts Together – what success will sound like
Our Experts Together Partnership, acting as the voice of local users of services, will ensure that we measure and deliver the outcomes in our plans.
We will seek everyone’s views, using a coproduced tool. When everyone who needs health and social care support feels and says what is set out below, then we will know we have made the difference.
“I have agreed care and support. Everyone works well together and with me”.
“I have care and support that see’s me as a unique person with my own skills, strengths, and goals”.
“I can get information on how to keep myself fit and healthy”.
“I am supported to plan ahead for important changes in my life that I expect to happen”.
“I feel safe”.
“I have care and support that lets me live how I want to live”.
“I can get information and advice about my health and support”.
“I can get information on how to look after my overall wellbeing”.
“When I change services, there is a plan for what happens next and who does what”.
“I am supported to understand any risks and keep myself safe”.
The tools that we will use to enable us
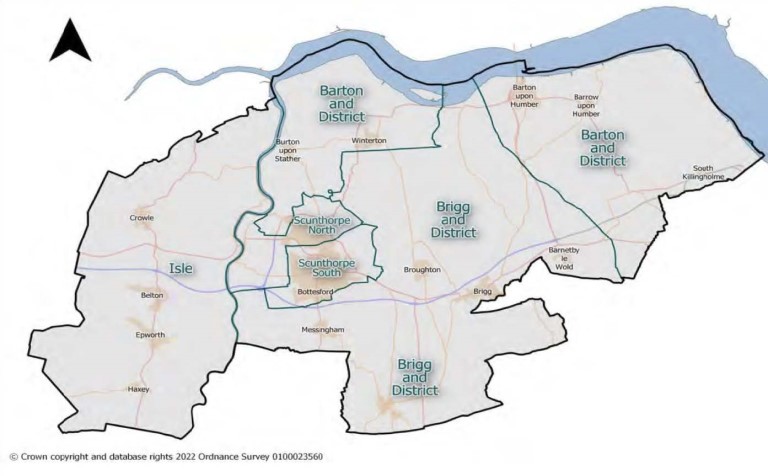
Our plans to develop Integrated Neighbourhood Teams, Integrated Urgent Care and Integrated Strategic Commissioning & Safeguarding will be designed to meet people’s need at the lowest level, with those most in need being prioritised. A single Neighbourhood based Planning Tool based on our population management approach will be used by all the organisations to understand need and inform proactive approaches to designing and delivering support that will improve people’s health and wellbeing. This means that care and support can be better tailored to meet people’s need, health and care services will be more joined-up and better use of public resources will be achieved. This Planning Tool will enable the needs of people in North Lincolnshire to be understood as a single area (172,000 people), Neighbourhood (around 40,000 people) or Lower Super Output Area (LSOA around 1,750 people). And importantly it will enable us to place every individual person at the centre of the tailored, personalised care that they need. The five Neighbourhoods the Planning Tool is based on is shown below.
Locality
| Locality | Population |
|---|---|
| Barton and District | 34, 498 |
| Brigg and District | 30,952 |
| Isle comprising | 23,298 |
| Scunthorpe North | 28,106 |
| Scunthorpe South | 55,894 |
| North Lincolnshire | 172,748 |
In addition to a single Planning Tool, there are five other tools, or enablers, that will be used. These are set out below.
A Single Workforce Strategy will enable everyone working within health and social care to share the same collaborative ambition, Strategic Intent and Community First Approach.
Strategic workforce planning will train and develop the workforce, enhance a mobile and transferable workforce, offer clear professional development opportunities and progression pathways. This will support recruitment and retention.
Shared systems and processes will be developed which will underpin a common language and a common identity. This will also help create joint accountability and drive integration. We will use data, insight and digital innovation to enable and support the workforce to be and do the best that we all can.
Inclusive and compassionate leadership will embed mutual respect, enhancing equality, diversity and inclusion within the workforce. Workforce wellbeing and engagement will foster a culture of one team and a team of teams, where everyone in the workforce feels:
- Safe to be themselves
- Well, resilient and highly motivated
- Valued and engaged, and
- Connected and high performing.
Digital Enablement and Innovation will help people to get digitally enabled care where this is the right thing for them, facilitate greater integration and co-production across all organisations involved in health and social care and support the design of preventative, personalised care for those that need it.
Collective Use of Resources will ensure that the money, people, assets, expertise, experience and leadership that North Lincolnshire has are put to the best, most effective and efficient use. We have agreed a single Place based approach with all partners to capital planning and estates utilisation that will enable the best use of our facilities and resources.
Strong Organisational Change and Transformational Change Management Approaches will make sure that the difference is achieved and continually delivers even better health and wellbeing outcomes for everyone in North Lincolnshire. Understanding each other’s team structures and ways of working and establishing shared values, behaviours, understanding, vision and agreements all contribute to this, with clear and joint accountability by all partners.
Sustainability will be at the heart of all that we do. We will take responsibility and enable positive action on the environment. We will make sure our Community First Transformation is safe for the environment, self-sustaining and provides opportunities for everyone by connecting people with nature so they benefit from improved health and well-being.


In Summary… Community First – Making It Real
Community First will enable people and ensure that they get the right care, in the right place at the right time. Based on prevention and enabling self-help, people will be able to act to keep themselves well. We will make it easy for communities to help people in ways that reduces their need for more health or social care and support, through offering services that meet need, enabling communities and building the right capacity within communities. People and their families will be empowered to support themselves and self-responsibility for wellbeing will be encouraged.
When people have a need for more health and social care support, people will get the best care, closest to home. This care will be personalised and will be provided in a way that ensures people have control over their lives.
Everyone involved in community wellbeing, health and social care will work together and seamlessly to ensure people’s needs are met. People who are most in need will be prioritised.
Adam’s story
Community First will make a difference to everyone who needs support, in the same way that Adam’s story makes a difference for him and his family. The following describes the difference our approach to integration will make.
Adam is a 37 year old with Autism and learning disabilities who has asthma, for which he had had repeated attendance at A&E.
He previously lived with parents, now he is in his own supported living flat.
In the past six months he had started to have increasing episodes of aggression and caused substantial damage to his property and which is leaving him very distressed.
His care provider felt that they could no longer safely meet his needs and gave notice on his care package. This was therefore offered to other local care providers, none of whom felt confident to meet his needs. Given there were no local options, an out of area placement was sought. This resulted in him being moved to a residential placement in Leeds due to the need to find a placement within a week.
He is moved within one week of the agreement of the plan.
This has impacted family visits and Adam is distressed. Family are concerned about his recovery, health and wellbeing.
There are routine case management visits to review his care, but Adam won’t engage. No formal or CQC concerns, but the staff don’t seem to have a good relationship with Adam and incidents and restraints have increased. This is causing further distress to Adam.
He has attended the Emergency Department several times due to poorly controlled asthma and self injury.
Adam has a Care and Treatment Review planned for next month.
Adam has been identified as having enhanced needs by the Integrated Neighbourhood Team.
He has appropriate support to manage his asthma. He’s getting gaining confidence and has an easy read care plan to help him.
The team have undertaken a holistic needs assessment with him and taken a personalised approach to meeting his needs.
The team also used social prescribing to ensure Adam is able to participate in community activities and volunteering opportunities. They work with a provider who feel the additional activities would help Adam feel his days have purpose and identify a range of offers for Adam in his local community. Adam’s support team accompany him to his choice of activities, spread throughout the week. Adam starts to look forward to these sessions and is volunteering at the local charity shop with a view to seeking employment. The team note he is much improved, he has more confidence in managing his asthma, and he says he feels happier because he can get out and do activities.
Recently, Adam’s needs have become more complex.
Due to the strong provider engagement in North Lincolnshire, there is ongoing partnership covered collaboration between the provider and other agencies across North Lincolnshire to ensure staff have the skills and competences to manage Adams increasing needs.
Staff in his supported living accommodation have been trained to recognise early any deterioration and to contact the North Lincolnshire Complex Care Team to discuss how best to support him.
The team advise and put in place some additional positive behavioural support to help manage Adam’s increasing agitation. The staff at his supported living accommodation also increase their imports to help Adam with emotional regulation. They have shared risk plan on access to support from the MDT 24/7 to support him remain at home.
Adam responds well and although occasionally aggressive he’s not violent and he’s managing his behaviour. There is greater understanding around Adam’s communication and the environment is adjusted to be conducive to meeting his needs. This includes adjustments and use of technology to support sensory needs.
He is now safely supported at home.
Adam’s Integrated Neighbourhood Team work closely together to ensure Adam understands his asthma and how to take his inhalers. But this doesn’t mean Adam never gets ill. Last week he got extremely breathless. He finds his frightening and worried that he needed to go to hospital. Adam has always been frightened of hospitals. However his support workers know how to help him. His support work around the local single point of access, where they spoke to a clinician who gave immediate advice. It was agreed that Adam needed to be seen in the Urgent Care Service for a full assessment and treatment – it was agreed the support worker could take him there to reduce Adam’s anxiety about hospitals.
On arrival, Adam is taken to the Urgent Care Service in the emergency department and assessed. He needed investigations, however it was agreed that he should be managed on the same day emergency care (SDEC) with a plan to get him home the same day. On SDEC, he’s treated quickly and start to show signs of improvement. Discharge planning starts immediately to reduce the time Adam needs to be spend in hospital. His support worker stays with him and this helps his anxiety. The Hospital Discharge Team have access to all the information they need to ensure he can be discharged with the support he needs in place. The community team schedule a visit to visit him at home the following day.
He’s discharged from SDEC the same day.
Next steps
Detailed action plans that identify how we will deliver our aspirations are being coproduced by all health and social care partners. Together with clear leadership arrangements for delivery of our plans across our Place partners, these action plans will be regularly reviewed with quarterly summary reports being presented to the Health and Wellbeing board as it progresses.